Personalized medicine is hoping to reach new heights thanks to the Cancer Moonshot, but won't get off the ground without a community-wide commitment to sharing big data.
The precision medicine community has long since recognized that sharing big data, including clinical records, genomic sequencing data, community-level health indicators, and research results, will be critical to making progress against cancer, neurodegenerative diseases, inherited conditions, and expensive chronic diseases like diabetes.
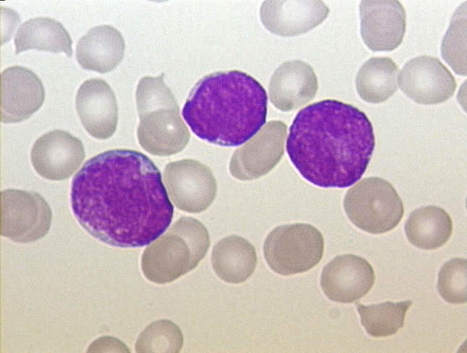
“Why is data sharing important? Because cancer is complex,” said Kenneth C. Anderson, MD, President-elect of the American Society of Hematology (ASH). Anderson specializes in multiple myeloma, a blood cancer with treatment options that hinge on the genetic variances of each and every patient.
“We’re learning so much about cancer, and applying these insights to drug development has been incredibly fruitful,” he continued. “Now we have treatments that are specifically targeted to patients’ genetic mutations. Not only are these treatments more effective — because they correct a specific mutation — they also minimize harmful side effects that we see with traditional total-body anticancer medicines.”
However, the continued development of these treatments cannot be sustained without a commitment to data sharing, he added.
more at http://healthitanalytics.com/news/why-sharing-cancer-big-data-is-key-to-personalized-medicine



 Your new post is loading...
Your new post is loading...