Your new post is loading...
 Your new post is loading...

|
Scooped by
nrip
|
Health IT can only be an enabler in vaccination drives. The right technology applications can turn the COVID-19 vaccination program into a game-changer for the healthcare industry To effectively digitize the immunization process, it is important to map all workflows and stakeholders of the immunization platform or application being used. The primary stakeholders in a vaccination program include the patient, the physician, the vaccination administrator and the public surveillance authorities who track vaccine administration and efficacy, especially in an outbreak. Some of the intervention points where technology can be an enabler in vaccine administration include: -
Vaccine tracking. Maintaining the cold chain for vaccines is an important activity, especially when vaccines are transported over long distances and require storage under specified conditions. Tracking technologies include sensors to monitor the temperature of the vials and dashboards to track the supply chain logistics across various distribution channels. -
Searching for vaccine providers. Vaccine finders are simple web portals for conveniently locating appropriate providers in the vicinity. For COVID-19, the CDC is currently managing this web portal and lists the vaccination centers and providers across the country. -
Checking eligibility. Most countries use a staggered approach to administer vaccines, with the more vulnerable receiving the doses earlier. A simple checklist or a questionnaire on the web portal can help people know about their eligibility based on the public health services guidelines. -
Scheduling a vaccination. This works like any other scheduling protocol, like scheduling an appointment, and can help avoid overcrowding at vaccination centers. -
Communication. There is some amount of vaccine hesitancy across the globe, and every government is making substantial efforts to allay the fears of the masses through social media campaigns, chatbots, help-line numbers and other means. -
Vaccination Reports/Passports Communicating the vaccination status of an individual with a digital report is an important part of the COVID vaccination drive. Several nations are debating the use of digital health certificates with vaccination QR codes to permit admission to their countries. QR code-based vaccination certificates can be saved on mobile phones and allow public health authorities to track vaccine drives and authenticate vaccine vials, and thereby inventories. The certificate does not disclose any personal health information. -
Data reporting and analytics. Large-scale vaccination programs are monitored by automated reports for the public health administrators. Technology around vaccination workflows, especially in the current scenario, where a large population must be vaccinated, could be a deterrent if not implemented correctly. The following steps must be taken to ensure technology is an enabler for this immunization drive: -
Create simple, intuitive interfaces that are usable across all age groups and demographics. -
Consider all workflows and map touchpoints of all stakeholders, including vaccinators, users and public health officials, to the actual interaction. -
Support ease of integration into the EMR to allow patient data to be enriched with immunization records. The QR codes in vaccination information statements allow scanning the code into EMRs, immunization information systems or other electronic devices. read more at https://www.healthcareitnews.com/blog/how-optimize-health-it-systems-immunization-drives

|
Scooped by
nrip
|
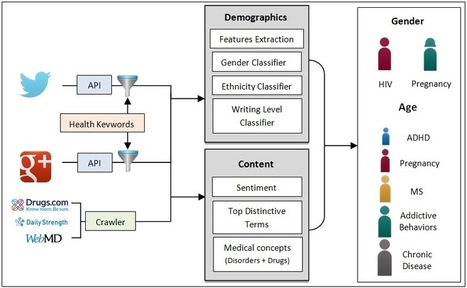
As Web-based social media are growing in popularity, the number of people who share their experiences or ask for support in health-related social media has also increased. A study found that 41% of e-patients have read someone else’s commentary or experience about health on a Web-based news group, website, or blog. Another study reported that more than 60 million Americans read or contribute to Health 2.0 apps, in which they consider these apps as their first source when gathering data and opinions. About 40% of Americans doubt a professional opinion when it conflicted with what they form from Web-based health social media. One of the key benefits of health-related Web-based social media reported by researchers is the increased access to information to various demographic groups, regardless of age, education, income, or location. However, previous work has mainly relied on user surveys to study the effect of the use of social media to health-related factors such as psychological distress. In addition, previous work does not reveal granular information on what disorders or other health topics are mostly discussed in the Internet by each demographic group, which would allow health care providers to create targeted and effective educational campaigns. In this work, we conducted the first, to our best knowledge, large-scale data-driven comparative analysis of the content of health-related social media across various demographic dimensions—gender, age, ethnicity, location, and writing level. For each demographic group, we study the content of the posts across the following dimensions: sentiment, popular terms (keywords), and medical concepts (particularly disorders and drugs). Concepts refer to entries in the Unified Medical Language System (UMLS) vocabulary, whereas terms are just words from the posts’ text that may or may not belong to any UMLS concept. We report results for 3 types of social media: (1) general Web-Based Social Networks, namely Google+ and Twitter, (2) drug review websites, and (3) health Web forums. The selection of social media types was based on their popularity and on our study of the literature on health-related social content. The objective of this study was to identify which health topics are discussed in which social media by which demographic groups, to better guide educational outreach and research activities. read the whole study at http://www.jmir.org/2016/6/e148/

|
Scooped by
nrip
|
Current controversy surrounding health domains is rooted in the Internet’s growing importance as a health information source. In 2013, the International Telecommunication Union estimated that 38.8% (2.7 billion) of the world’s population used the Internet. Many of these users are seeking important health information online. In the United States, surveys report 72% of online adults accessed the Internet to find health information primarily on the subjects of diseases and treatments . Other regions, including the European Union and emerging markets, have also shown marked increases in online health information seeking and self-diagnosing behavior.
The importance of establishing an inclusive yet reliable presence for health information online is critical to future global health outcomes given the growing importance of the health Internet. However, .health and many other health-related gTLDs are now on sale to private sector entities that largely permit open and unrestricted use. Yet, the globalized nature of the Internet, the public health need for privacy, security, and quality health information, and the rapid expansion of online health technologies demonstrate a critical need to ensure proper governance of future health domains. Focusing on the public good can be a first and crucial step to ensure an accurate, reliable, and evidence-based online presence for health for this generation and the next.

|
Scooped by
nrip
|
Patient engagement represents the next aim of healthcare reform through the adoption of health IT systems and services. It just received a boost from PCORI which awarded $93.5 million for the creation of 29 clinical research data networks that will combine to form its National Patient-Centered Clinical Research Network (PCORnet).
A major aim of establishing these networks is to enable the patient population to play an active role in how their care is delivered. “One of the reasons people think we should be engaging patients more actively is to make sure that as we do research we’re measuring and assessing the kinds of things they want to know when they’re making medical decisions,” says Elizabeth McGlynn, PhD, Director of the Center for Effectiveness & Safety Research at Kaiser Permanente.
“While we appreciate that more traditional biometric information may be important,” she continues, “there are a number of other things that any of us who have had to make decisions about whether or not to have a surgical procedure or take a particular drug would like to know beyond some of that information.” McGlynn and her team of researchers will rely on its network, Partners Patient Outcomes Research To Advance Learning (PORTAL), to change how a healthcare organization learns from its patients, namely in bridging the gap between the latter and researchers. “The whole area of engaging patients more actively and comprehensively in research is an evolving one.
At a high level, the challenges for the project are two-fold. On the one hand, researchers need to be able to understand how patients want to be engaged:
We know that patients aren’t homogenous; we know that there’s a range of opinion. These kinds of tools give us the chance to continue to appreciate the diversity of ideas and opinions and avoid trying to just get to the one or the two leading ideas but really to think. As people are exploring the notion of what personalized medicine means, how do we make sure that we’re eliciting information from people about what’s important to them personally?
On the other hand, they must tackle the challenge of making this feedback available to clinicians in a meaningful way:
One of our big challenges is finding ways to effectively integrate that information into the electronic health record. We have some work underway right now that’s given us some early insights into what patients are willing to provide if their doctors are going to see it and use it but if it’s just a hypothetical exercise, not so interested.

|
Scooped by
nrip
|
Each of our bodies is utterly unique, which is a lovely thought until it comes to treating an illness -- when every body reacts differently, often unpredictably, to standard treatment. Tissue engineer Nina Tandon talks about a possible solution: Using pluripotent stem cells to make personalized models of organs on which to test new drugs and treatments, and storing them on computer chips. (Call it extremely personalized medicine.)
There are lots of medical apps available for smart phones and tablets, many of which are free or inexpensive. But how do you incorporate them into clinical practice?
The good news is you don’t have to invest in fancy equipment. If you’re asking about apps, you probably own a smart phone or tablet. Your patients who will benefit most from apps own the technology already, too. So the most efficient and effective way to start is to use the technology you have, and have learners use what they have.
Next step is to find the most appropriate resources. Do not start from “what apps are available?” That would not be patient-centered. Instead, ask: What conditions do my patients have? What do I teach about? What do my patients and their families need to learn? What questions do they have? What behaviors do they need help changing to optimize health?
There are 3 places apps might be used:
1. In the clinical encounter, as you explain something.
2. During a hospitalization, to engage the patient and family in the educational process.
3. At home, to provide information and support healthy behavior changes.
Read more: http://notimetoteach.com/2013/using-apps-to-enhance-patient-and-family-education/
Via Parag Vora

|
Scooped by
nrip
|
Patient engagement, defined as the process of placing patients at the center and in control of their own healthcare, is becoming a chief healthcare priority
Concurrently, a number of national information infrastructure initiatives are targeting increased patient engagement and the design of health information systems that improve the availability of health information and integrate it in meaningful ways for patients. So far, these technology goals have been advanced primarily through the design of personal health records (PHRs), patient portals, electronic health records (EHRs), and health information exchanges (HIEs). However, we remain far from achieving the goal of truly engaging patients in their care.
Generation and exchange of health data with patients is a requirement for Stage 3 EHR meaningful use incentives. Patients are entitled to an electronically generated copy of the record of their encounters with providers.
Sharing provider-generated data with patients is expected to promote patient engagement and accountability, but our own experiences suggest that the data that are being shared are currently a mixed blessing. For example, one encounter report took the form of a 6-page document in which the vast majority of information was copied and pasted from previous encounters and in which there were several factual errors. The errors will be discussed with the provider during the next visit.
Certainly the report got our attention; whether empowerment will result remains an open question. On another occasion, although the visit itself had included making decisions about future treatment, the plan was not mentioned in the document, leaving the patient to rely on her own memory and notes. The National eHealth Collaborative Technical Expert Panel recommends fully integrating patient-generated data (e.g., home monitoring of daily weights, blood glucose, or blood pressure readings) into the clinical workflow of healthcare providers
Although patients want this type of involvement, we have only begun to address their wishes and concerns. In the next sections, we summarize the current status of several potential building blocks to achieving patient engagement goals and emphasize the role of the nurse informaticist as fundamental to the process.
more at the original : http://ojni.org/issues/?p=2848
|

|
Scooped by
nrip
|
The Ministry of Health and the Ghana Health Service has engaged the services of Lightwave ehealthcare Services (LWEHS) to roll out an integrated health care solution that includes a Centralized data center with a 24 hour recovery unit to serve as an infrastructure platform for a patient-centered health care solution. The solution will network all health facilities including agencies of the Ministry of Health, provide electronic Medical records for care seekers, enable and facilitate tele medicine, and develop a a real time bio-surveillance system – which will support the fight against disease outbreaks and the spread of communicable disease. The system which integrates with the current National Health Insurance Scheme (NHIS) enables the development of a patient management system – this will streamline the Admission, discharge and transfer process of healthcare. Chief Technology Officer of Lightwave Mr Thomas Mac Scofield, said the project was a culmination of years of planning and working with the MOH to bring ehealth solutions to the public health care industry. Mr Thomas Mac Scofield revealed to Ghanahealthnest.com that, the cost of the project is covered by the government through the MoH and GHS thus will not require patients or subscribers to pay for it. Nrip Nihalani consulting director with LightWave revealed to Ghanahealthnest.com that the project follows Ghana’s Data privacy and HIPAA laws to ensure its safety. He added that, the time was right for Ghana as most countries have gone ahead and made significant mistakes. “Ghana is at the absolute time with the technologies, the budgets, the preparedness all meeting together to launch its e-health”, Nrip intoned. more at : http://ghanahealthnest.com/nationwide-paperless-ehealth-project-commenced-ghana/

|
Scooped by
nrip
|
Many recent headlines regarding DNA and genetic science have been complex and hard for the average person to relate to. When the technology saves a young person's life, such as what happened recently at the University of California, San Francisco, the science takes on human qualities, and as a public, we can truly grasp just how important and revolutionary this combination of biology and technology really is.
Dr. James Gern, a professor of pediatrics and medicine at the University of Wisconsin School of Medicine and Public Health in Madison, contacted Joseph DeRisi for help after his patient, a 14-year-old boy, was hospitalized with encephalitis. The prognosis was so severe that the young man had been hospitalized for six weeks and put into a medically induced coma, according to a press release.
None of the tests and procedures run so far had managed to point out the cause of the boy’s illness. Gern contacted DeRisi, chair of biochemistry and biophysics at UCSF, due to his expertise in new genomic techniques. These techniques involved identifying pathogens that were previously unknown, such as that which caused the young man's illness. According to DeRisi, with this new technology, essentially any pathogen can now be detected with a single test. Once the cause was found, correct treatment could be administered.
The case study can be found published online in the New England Journal of Medicine.
Using SURPI, a tool used in “next generation-sequencing,” a team of researchers quickly and efficiently found the cause of the young man’s illness. With the help of the technology, the team compared samples of the boy’s DNA to the GenBank databases maintained by the National Center for Biotechnology Information with awe-inspiring speed, doing in 96 minutes what before took at least a day. Researchers determined that 475 distinct DNA sequences among the three million DNA sequences obtained in the patient’s cereospinal fluid came from a type of bacteria called Leptospira.
The team was even able to pinpoint the exact strain of Leptospira that they boy had been contaminated with: one native to the Caribbean and warmer climates.
Based on these findings, researchers decided to treat the boy using penicillin without having the diagnosis validated with a clinically approved test.
The antibiotics treatment was successful in ridding the boy’s body of infection, and he was discharged and sent home shortly afterward.
Validation by a clinically approved test could have taken upward of five months to confirm, and by this time the boy may not have survived.
more at http://www.medicaldaily.com/dna-sequencing-test-saves-young-teens-life-technology-just-months-away-commercial-approval-286490
The case study can be read at http://www.nejm.org/doi/full/10.1056/NEJMoa1401268#t=article

|
Scooped by
nrip
|
Commonwealth Fund researchers analyzed data from surveys of primary care physicians conducted in 2009 and 2012 to check on the progress of health IT adoption.
Adoption of health information technology (HIT) by physician practices rose considerably from 2009 to 2012, yet solo physicians lag practices of 20 or more and certain functions—like electronically exchanging information with other physicians—have been adopted by only a minority of providers. Physicians who are part of an integrated delivery system, share resources with other practices, and are eligible for financial incentives, have higher rates of HIT adoption.
Doctors are using HIT in greater numbers, spurred on in part by the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009, which provided billions to help build a national HIT infrastructure. Commonwealth Fund researchers analyzed data from surveys of primary care physicians conducted in 2009 and 2012 to check on the progress of HIT adoption and to see how certain factors—like being part of an integrated health system or using shared technical assistance programs—can influence technology take-up. Key Findings - From 2009 to 2012, the rate of adoption of electronic medical records (EMRs) by U.S. primary care physicians increased by half, from 46 percent to 69 percent. HIT use rose particularly in order entry management: the proportion of physicians able to send prescriptions electronically to pharmacies nearly doubled, from 34 percent to 66 percent; electronic prescribing increased from 40 percent to 64 percent; and electronic ordering of lab tests grew from 38 percent to 54 percent.
- In 2012, 33 percent of primary care physicians could exchange clinical summaries with other doctors, and 35 percent could share lab or diagnostic tests with doctors outside their practice.
- As of 2012, a minority of physicians provided electronic access for patients. Roughly one-third or fewer allowed patients to electronically view test results, make appointments, or request prescription refills.
- Practice size is a major determinant of HIT adoption. Half of physicians in solo practices use EMRs, compared with 90 percent of those in practices of 20 or more physicians.
- Physicians who are part of an integrated delivery system (like Kaiser Permanente or the Veterans Administration), those who have arrangements with other practices to share resources (technical assistance programs for clinical information systems or quality improvement), and those who are eligible for financial incentives, have higher rates of HIT adoption.
more at http://www.commonwealthfund.org/Publications/In-the-Literature/2014/Jan/Where-Are-We-on-the-Diffusion-Curve.aspx

|
Scooped by
nrip
|
You walk in to the doctor’s office – nervous – thinking of the last time you received the injection of your monthly medication, remembering how painful and aggravating it was when the nurse couldn’t find your vein and poked you five different times to insert the IV.
This time, however, something is different. When the nurse shows up he is wearing a special pair of glasses, something you wouldn’t expect to see during such a standard procedure. The device uses advanced technology and shows the nurse a perfect highlighted image of your veins so he can insert the IV in one painless attempt.
Sounds like science fiction right? Wrong. This is a real device and is just one early example of how Augmented Reality (AR) technology is changing the healthcare landscape.
Research shows that up to 40 percent of IV sessions require multiple attempts to locate and access the vein. Augmented reality comes to the rescue in a standard procedure that still causes so much discomfort and dissatisfaction.
Typically, when people think of AR, they imagine glasses and screens that present new layers of content on top of real world images. This traditional model will still play a significant role in the future. However, there’s another aspect to AR that will be important, specifically in the healthcare industry and that is the ability to instantly display relevant information to people who need it most.
Imagine a doctor who is able to view a patient’s medical history displayed over the latest medical scan, and even over the patient himself. We are already beginning to see wearable medical devices that provide critical health information during relevant points of the day.
In the near future, the next time you want to bite into your hamburger, you might get a friendly reminder that your cholesterol level won’t like it. Overcoming roadblocks with the help of the crowd We are still facing significant barriers before we will be able to see AR’s full potential in action. Some of these barriers are practical, such as problems with Wi-Fi connectivity and battery life. Several of the barriers are conceptual, but we do see a huge shift in people’s mindsets. Wearables will play a major role in this. For example, there have been several crowd-sourced campaigns to develop wearables that could sense your heart rate and blood oxygen levels and send you real-time notifications. In another case, there was an abdominal surgery that took place on one side of a city, and in parallel was live-streamed via glasses to a medical school class. The right information to save lives Medicine is one of the industries that provides tangible real-world benefits to help people live better lives, and AR can help immensely. When you’re dealing with life and death decisions, immediate access to necessary and relevant information is of the utmost importance.
This is where AR has the most potential to disrupt the industry – putting the information doctors and healthcare providers need in front of their eyes, when they need it. Beyond that, this same experience can be tailored for the needs of patients and everyday users unlocking the potential for a real revolution in health and in the way people think about maintaining their health.
The field of medical technology is incredibly exciting these days. Each breakthrough has the potential to impact the lives of thousands of patients, sometimes changing the course of medical history and forever improving the human experience. Such can be argued for antibiotics, x-rays, vaccines, or even things as seemingly simple as disposable medical instruments (an extremely important sanitary innovation). Year after year, teams of research physicians and engineers work to advance our knowledge and abilities.
This article reviews some of the most influential medical innovations of the past year. From new insights in the treatment of diabetes to a new type of optical surgical procedure, incredible innovations and advancements have been achieved this year.
Implant Relieving Severe Headache Pain
A new type of neuromodulation therapy has emerged that seems to be an effective treatment for cluster and migraine headaches. Neuromodulation therapy treats a cluster of nerves behind the face that signal headache pain. This device, implanted in the face by way of the mouth, is positioned to stimulate the facial nerve that relieves headaches when stimulated. A separate device, placed on the cheek, activates the device, relieving pain in as quickly as five to ten minutes.
Bariatric Surgeries Treating Diabetes Doctors who have performed bariatric surgery, also known as gastric bypass, have noted in the past that many of their patients had gone into diabetes remission as they recovered from surgery. This evidence has some health care professionals advocating gastric bypass treatment as an early tactic for fighting diabetes, instead of as a last-resort effort.
Bee Venom Treats HIV One toxin found in bee venom, melittin, has been found to destroy HIV particles. Researchers claim that the particles break apart the physical structure of the virus, but are too small to have an impact on other cells within the body. A proposed method for distributing the chemical is a topical virucidal agent.
Detecting Skin Cancer with a Hand-held Device Caught at an early stage, the survival rate for melanoma is 99 percent. In advanced stages, though, that rate drops to a mere 15 percent. The good thing about the skin and its relation to cancer is that we can observe it. Visual detection is the best way to prevent advanced stage melanoma. Therefore checking moles and other discoloration on the skin regularly can be the best form of early detection. If a patient notices a change and brings it to the attention of their dermatologist, this new device is able to scan the area and report to the physician whether or not melanoma is present within a few seconds. It works by analyzing a database of over 10,000 images alongside a structural scan of the skin using military-grade optical technology. Clinical trials show that this device is nearly 98% effective.
Cataract Surgery at one Quadrillionth of a Second
Femtosecond laser technology will help improve the outcome in the more than 1.6 million annual cataract surgeries that are performed in the US annually. The apparatus, which separates the tissue by ablating and cleaving it, instead of cutting it, operates in one quadrillionth of a second. Its speed and precision help reduce swelling post-op, allow less time to be spent on the eye, and help the surgeon be more accurate with the implant. Optical surgeons across the globe are eager to implement this new device in order to improve their practice.
More at the original at : http://medcitynews.com/2013/12/biggest-innovations-medical-technology-2013/
Via Parag Vora

|
Scooped by
nrip
|
A fundamental question about any (Clinical Decision Support System) CDS is just how good is it, i.e. does it get the right answer for generic and specific patients? If it doesn’t this may be the result of one or more issues such as flawed information having been used to build the system, flawed programming, or the patient being outside of an often undefined or ill defined population when for another population the CDS does actually provide the right answer
A common CDS disclaimer is that it is always up to the practitioner to second guess the CDS as necessary, or in other words, the CDS is not actually supposed to be relied upon. Depending on the complexity of the underlying theory and data, the practitioner may or may not in reality have the ability to do this, or they may not have a more rational basis for doing so than “I don’t think that is right”. Such a conclusion would put the practitioner outside of what might be considered a practice guideline. On the other hand if a CDS is easy to second guess, then it might not be very valuable in the first place.
In this context comes the recent controversy over the new cholesterol and statin on line “risk calculator”. As first reported in the New York Times, it was determined that an online risk calculator overestimated patient specific risk by an average of 100% (100 here is not a typo). If action were based on this erroneous calculator, statin therapy would be substantially over-prescribed. In this regard the Times cites a statement from the organizations that published the guidelines that will continue to be a CDS classic: patients and doctors should discuss treatment options rather than blindly follow a calculator. Or, in other words, it is not to be relied on.
Apparently the problem with the risk calculator is at least in part that the risk data on which it was based was decades old and therefore did not apply to the current US population which in at least some ways has actually gotten healthier. In addition the mathematical model used was one of linearly increasing risk which has not been demonstrated to be correct. Thus the flaws in the calculator were a result of the inappropriateness and lack of justification of the knowledge bases used to build it. Despite these fundamental issues, no plans to remove or revise the calculator were identified.
This risk calculator was not imbedded within an EHR, and it requires manual input of multiple patient parameters. And of course there are additional potentially relevant patient parameters that are not part of the calculation. However something like this certainly could be part of an EHR either by direct integration, or by pointing the EHR user to it and perhaps automatically using relevant patient information that might already be in the EHR.
more at http://www.hitechanswers.net/lesson-clinical-decision-support/
|



 Your new post is loading...
Your new post is loading...